Main Content
Adipocyte crosstalk within the tumor microenvironment
Research interests
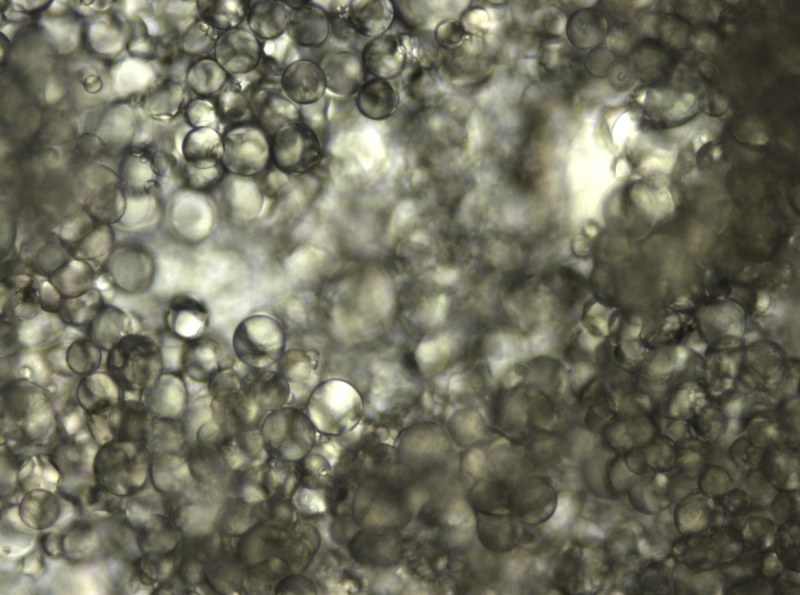
Far for being just a fat reservoir, adipose tissue is recognized as a true endocrine organ which orchestrates metabolic homeostasis in the whole organism. Currently, it is known that this inter-organ crosstalk is mediated not only by the release of ‘adipokines’ but also via extracellular vesicles (EVs). Notably, several studies have remarked adipose tissue as the main contributor of circulating EVs. EVs are nanometer-sized vesicles that are surrounded by a membrane and are used by virtually all cells to exchange signal molecules. It is hypothesized that under cellular stress conditions, as is the case for cancer, normal vesicular trafficking and protein and nucleic acid content are altered, creating an environment that aids cancer initiation, progression and metastasis. In obesity, adipocyte dysfunction leads to a meta-inflammatory state together with ectopic fat deposition, which altogether contributes to the development of several comorbidities including insulin resistance, cardiovascular disease and cancer. However, how adipocyte dysfunction and adipocyte-derived EVs are integrated into the obesity-cancer binomial is still poorly understood.
Within the tumour microenvironment (TME), adipocytes are transformed into so-called cancer-associated adipocytes (CAAs). De-differentiation of mature adipocytes and reprogramming into CAAs is a well-known event in cancer development, however the bulk of data has been generated from breast cancer and melanoma models, limiting the extension of conclusions to ovarian cancer (OC). OC is the fifth most common cancer in European females and the deadliest of all gynecological malignancies, with >60,000 new cases annually in the European Union and the United States and an overall 5-year survival rate of ~40%. Several features contribute to the fatal nature of OC, which distinguish it from other human cancers. These features concern primarily the role of peritoneal fluid in cancer cell spread within the abdominal cavity and that the omentum (a visceral protective adipose structure) constitutes the primary site of OC metastasis in contrast to other cancers. Recently, it has been described that EVs in the TME of OC (i.e., in ascites) carry numerous proteins associated with a short relapse-free survival, including molecules possibly derived from adipocytes. Moreover, tumor cells surviving chemotherapy can trigger disease recurrence by invading the peritoneum or omentum and establishing metastatic lesions. Conditional resistance is also modulated by interactions with host cells (such as adipocytes), which therefore represent an unexplored potential target to overcome therapy resistance. We believe that a better understanding of the ascites-driven reprogramming suffered by adipocytes in OC will help to design better therapeutic strategies.
In summary, our research group wants to deepen into the molecular changes suffered by adipocytes under stress conditions such as cancer-driven inflammation, and how these changes impact EV release and function. We hypothesise that CAA-derived EVs may exert a pro-tumorigenic role not only by affecting tumour cell growth and chemoresistance of cells but also by exerting an immunomodulation of other host cells such as macrophages or NK cells.
Other research projects
In addition to the biology of adipocytes and adipocyte-derived EVs, we are also interested in the application of state-of-the-art techniques for the analysis of EVs (like fluorescent nano-flow cytometry or proteomics) and the use of EVs as potential therapeutic approaches.
To this aim, we work on parallel projects including the development of recombinant EVs (in collaboration with AG Pogge) as well as the functional analysis of mesenchymal stromal cell-derived EVs as new therapeutic tools in inflammatory diseases (in collaboration with AG Casado in Spain).